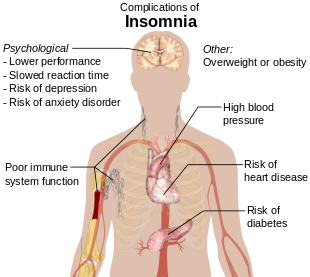
Insomnia, also known as sleeplessness, is a sleep disorder where people have trouble sleeping.[1] They may have difficulty falling asleep, or staying asleep as long as desired.[11][9] Insomnia is typically followed by daytime sleepiness, low energy, irritability, and a depressed mood.[1] It may result in an increased risk of motor vehicle collisions, as well as problems focusing and learning.[1] Insomnia can be short term, lasting for days or weeks, or long term, lasting more than a month.[1]
Insomnia can occur independently or as a result of another problem.[2] Conditions that can result in insomnia include psychological stress, chronic pain, heart failure, hyperthyroidism, heartburn, restless leg syndrome, menopause, certain medications, and drugs such as caffeine, nicotine, and alcohol.[2][8] Other risk factors include working night shifts and sleep apnea.[9] Diagnosis is based on sleep habits and an examination to look for underlying causes.[3] A sleep study may be done to look for underlying sleep disorders.[3] Screening may be done with two questions: “do you experience difficulty sleeping?” and “do you have difficulty falling or staying asleep?”[9]
Sleep hygiene and lifestyle changes are typically the first treatment for insomnia.[5][7] Sleep hygiene includes a consistent bedtime, exposure to sunlight, a quiet and dark room, and regular exercise.[7] Cognitive behavioral therapy may be added to this.[6][12] While sleeping pills may help, they are associated with injuries, dementia, and addiction.[5][6] Medications are not recommended for more than four or five weeks.[6] The effectiveness and safety of alternative medicine is unclear.[5][6]
Between 10% and 30% of adults have insomnia at any given point in time and up to half of people have insomnia in a given year.[8][9][10] About 6% of people have insomnia that is not due to another problem and lasts for more than a month.[9] People over the age of 65 are affected more often than younger people.[7] Females are more often affected than males.[8] Descriptions of insomnia occur at least as far back as ancient Greece.[13]
Contents
Signs and symptoms
Symptoms of insomnia:[15]
- difficulty falling asleep, including difficulty finding a comfortable sleeping position
- waking during the night and being unable to return to sleep
- feeling unrefreshed upon waking
- daytime sleepiness, irritability or anxiety
Sleep-onset insomnia is difficulty falling asleep at the beginning of the night, often a symptom of anxiety disorders. Delayed sleep phase disorder can be misdiagnosed as insomnia, as sleep onset is delayed to much later than normal while awakening spills over into daylight hours.[16]
It is common for patients who have difficulty falling asleep to also have nocturnal awakenings with difficulty returning to sleep. Two-thirds of these patients wake up in the middle of the night, with more than half having trouble falling back to sleep after a middle-of-the-night awakening.[17]
Early morning awakening is an awakening occurring earlier (more than 30 minutes) than desired with an inability to go back to sleep, and before total sleep time reaches 6.5 hours. Early morning awakening is often a characteristic of depression.[18]
Poor sleep quality
Poor sleep quality can occur as a result of, for example, restless legs, sleep apnea or major depression. Poor sleep quality is caused by the individual not reaching stage 3 or delta sleep which has restorative properties.[19]
Major depression leads to alterations in the function of the hypothalamic-pituitary-adrenal axis, causing excessive release of cortisol which can lead to poor sleep quality.
Nocturnal polyuria, excessive nighttime urination, can be very disturbing to sleep.[20]
Subjectivity
Some cases of insomnia are not really insomnia in the traditional sense. People experiencing sleep state misperception often sleep for normal durations, yet overestimate the time taken to fall and remain asleep.[21]
Causes
Symptoms of insomnia can be caused by or be associated with:
- Use of psychoactive drugs (such as stimulants), including certain medications, herbs, caffeine, nicotine, cocaine, amphetamines, methylphenidate, aripiprazole, MDMA, modafinil, or excessive alcohol intake.[22]
- Use of or withdrawal from alcohol and other sedatives, such as anti-anxiety and sleep drugs like benzodiazepines.[22]
- Use of or withdrawal from pain-relievers such as opioids.[22]
- Previous thoracic surgery.
- Heart disease.[23]
- Deviated nasal septum and nocturnal breathing disorders.[24]
- Restless legs syndrome, which can cause sleep onset insomnia due to the discomforting sensations felt and the need to move the legs or other body parts to relieve these sensations.[25]
- Periodic limb movement disorder (PLMD), which occurs during sleep and can cause arousals of which the sleeper is unaware.[26]
- Pain,[27] an injury or condition that causes pain can preclude an individual from finding a comfortable position in which to fall asleep, and can in addition cause awakening.
- Hormone shifts such as those that precede menstruation and those during menopause.[28]
- Life events such as fear, stress, anxiety, emotional or mental tension, work problems, financial stress, birth of a child, and bereavement.[25]
- Gastrointestinal issues such as heartburn or constipation.[29]
- Mental disorders such as bipolar disorder, clinical depression, generalized anxiety disorder, post traumatic stress disorder, schizophrenia, obsessive compulsive disorder, dementia,[30]:326 and ADHD.[31]
- Disturbances of the circadian rhythm, such as shift work and jet lag, can cause an inability to sleep at some times of the day and excessive sleepiness at other times of the day. Chronic circadian rhythm disorders are characterized by similar symptoms.[22]
- Certain neurological disorders, brain lesions, or a history of traumatic brain injury.[32]
- Medical conditions such as hyperthyroidism and rheumatoid arthritis.[33]
- Abuse of over-the counter or prescription sleep aids (sedative or depressant drugs) can produce rebound insomnia.[22]
- Poor sleep hygiene, e.g., noise or over-consumption of caffeine.[22]
- A rare genetic condition can cause a prion-based, permanent and eventually fatal form of insomnia called fatal familial insomnia.[34]
- Physical exercise. Exercise-induced insomnia is common in athletes in the form of prolonged sleep onset latency.[35]
Sleep studies using polysomnography have suggested that people who have sleep disruption have elevated nighttime levels of circulating cortisol and adrenocorticotropic hormone. They also have an elevated metabolic rate, which does not occur in people who do not have insomnia but whose sleep is intentionally disrupted during a sleep study. Studies of brain metabolism using positron emission tomography (PET) scans indicate that people with insomnia have higher metabolic rates by night and by day. The question remains whether these changes are the causes or consequences of long-term insomnia.[33]
Substance-induced
Alcohol-induced
Alcohol is often used as a form of self-treatment of insomnia to induce sleep. However, alcohol use to induce sleep can be a cause of insomnia. Long-term use of alcohol is associated with a decrease in NREM stage 3 and 4 sleep as well as suppression of REM sleep and REM sleep fragmentation. Frequent moving between sleep stages occurs, with awakenings due to headaches, the need to urinate, dehydration, and excessive sweating. Glutamine rebound also plays a role as when someone is drinking; alcohol inhibits glutamine, one of the body’s natural stimulants. When the person stops drinking, the body tries to make up for lost time by producing more glutamine than it needs. The increase in glutamine levels stimulates the brain while the drinker is trying to sleep, keeping him/her from reaching the deepest levels of sleep.[36] Stopping chronic alcohol use can also lead to severe insomnia with vivid dreams. During withdrawal REM sleep is typically exaggerated as part of a rebound effect.[37]
Benzodiazepine-induced
Like alcohol, benzodiazepines, such as alprazolam, clonazepam, lorazepam, and diazepam, are commonly used to treat insomnia in the short-term (both prescribed and self-medicated), but worsen sleep in the long-term. While benzodiazepines can put people to sleep (i.e., inhibit NREM stage 1 and 2 sleep), while asleep, the drugs disrupt sleep architecture: decreasing sleep time, delaying time to REM sleep, and decreasing deep slow-wave sleep (the most restorative part of sleep for both energy and mood).[38][39][40]
Opioid-induced
Opioid medications such as hydrocodone, oxycodone, and morphine are used for insomnia that is associated with pain due to their analgesic properties and hypnotic effects. Opioids can fragment sleep and decrease REM and stage 2 sleep. By producing analgesia and sedation, opioids may be appropriate in carefully selected patients with pain-associated insomnia.[27] However, dependence on opioids can lead to long-term sleep disturbances.[41]
Risk factors
Insomnia affects people of all age groups but people in the following groups have a higher chance of acquiring insomnia.[citation needed]
- Individuals older than 60
- History of mental health disorder including depression, etc.
- Emotional stress
- Working late night shifts
- Traveling through different time zones[11]
Mechanism
Two main models exists as to the mechanism of insomnia, (1) cognitive and (2) physiological. The cognitive model suggests rumination and hyperarousal contribute to preventing a person from falling asleep and might lead to an episode of insomnia.
The physiological model is based upon three major findings in people with insomnia; firstly, increased urinary cortisol and catecholamines have been found suggesting increased activity of the HPA axis and arousal; second increased global cerebral glucose utilization during wakefulness and NREM sleep in people with insomnia; and lastly increased full body metabolism and heart rate in those with insomnia. All these findings taken together suggest a dysregulation of the arousal system, cognitive system, and HPA axis all contributing to insomnia.[42][43] However, it is unknown if the hyperarousal is a result of, or cause of insomnia. Altered levels of the inhibitory neurotransmitter GABA have been found, but the results have been inconsistent, and the implications of altered levels of such a ubiquitous neurotransmitter are unknown. Studies on whether insomnia is driven by circadian control over sleep or a wake dependent process have shown inconsistent results, but some literature suggests a dysregulation of the circadian rhythm based on core temperature.[44] Increased beta activity and decreased delta wave activity has been observed on electroencephalograms; however, the implication of this is unknown.[45]
Around half of post-menopausal women experience sleep disturbances, and generally sleep disturbance is about twice as common in women as men; this appears to be due in part, but not completely, to changes in hormone levels, especially in and post-menopause.[28][46]
Changes in sex hormones in both men and women as they age may account in part for increased prevalence of sleep disorders in older people.[47]
Diagnosis
In medicine, insomnia is widely measured using the Athens insomnia scale.[48] It is measured using eight different parameters related to sleep, finally represented as an overall scale which assesses an individual’s sleep pattern.
A qualified sleep specialist should be consulted for the diagnosis of any sleep disorder so the appropriate measures can be taken. Past medical history and a physical examination need to be done to eliminate other conditions that could be the cause of insomnia. After all other conditions are ruled out a comprehensive sleep history should be taken. The sleep history should include sleep habits, medications (prescription and non-prescription), alcohol consumption, nicotine and caffeine intake, co-morbid illnesses, and sleep environment.[49] A sleep diary can be used to keep track of the individual’s sleep patterns. The diary should include time to bed, total sleep time, time to sleep onset, number of awakenings, use of medications, time of awakening, and subjective feelings in the morning.[49] The sleep diary can be replaced or validated by the use of out-patient actigraphy for a week or more, using a non-invasive device that measures movement.[50]
Workers who complain of insomnia should not routinely have polysomnography to screen for sleep disorders.[51] This test may be indicated for patients with symptoms in addition to insomnia, including sleep apnea, obesity, a thick neck diameter, or high-risk fullness of the flesh in the oropharynx.[51] Usually, the test is not needed to make a diagnosis, and insomnia especially for working people can often be treated by changing a job schedule to make time for sufficient sleep and by improving sleep hygiene.[51]
Some patients may need to do an overnight sleep study to determine if insomnia is present. Such a study will commonly involve assessment tools including a polysomnogram and the multiple sleep latency test. Specialists in sleep medicine are qualified to diagnose disorders within the, according to the ICSD, 81 major sleep disorder diagnostic categories.[52] Patients with some disorders, including delayed sleep phase disorder, are often mis-diagnosed with primary insomnia; when a person has trouble getting to sleep and awakening at desired times, but has a normal sleep pattern once asleep, a circadian rhythm disorder is a likely cause.
In many cases, insomnia is co-morbid with another disease, side-effects from medications, or a psychological problem. Approximately half of all diagnosed insomnia is related to psychiatric disorders.[53] In depression in many cases “insomnia should be regarded as a co-morbid condition, rather than as a secondary one;” insomnia typically predates psychiatric symptoms.[53] “In fact, it is possible that insomnia represents a significant risk for the development of a subsequent psychiatric disorder.”[9] Insomnia occur in between 60% and 80% of people with depression.[54] This may partly be due to treatment used for depression.[54]
Determination of causation is not necessary for a diagnosis.[53]
DSM-5 criteria
The DSM-5 criteria for insomnia include the following:[55]
Predominant complaint of dissatisfaction with sleep quantity or quality, associated with one (or more) of the following symptoms:
- Difficulty initiating sleep. (In children, this may manifest as difficulty initiating sleep without caregiver intervention.)
- Difficulty maintaining sleep, characterized by frequent awakenings or problems returning to sleep after awakenings. (In children, this may manifest as difficulty returning to sleep without caregiver intervention.)
- Early-morning awakening with inability to return to sleep.
In addition,
- The sleep disturbance causes clinically significant distress or impairment in social, occupational, educational, academic, behavioral, or other important areas of functioning.
- The sleep difficulty occurs at least 3 nights per week.
- The sleep difficulty is present for at least 3 months.
- The sleep difficulty occurs despite adequate opportunity for sleep.
- The insomnia is not better explained by and does not occur exclusively during the course of another sleep-wake disorder (e.g., narcolepsy, a breathing-related sleep disorder, a circadian rhythm sleep-wake disorder, a parasomnia).
- The insomnia is not attributable to the physiological effects of a substance (e.g., a drug of abuse, a medication).
- Coexisting mental disorders and medical conditions do not adequately explain the predominant complaint of insomnia.
Types
Insomnia can be classified as transient, acute, or chronic.
- Transient insomnia lasts for less than a week. It can be caused by another disorder, by changes in the sleep environment, by the timing of sleep, severe depression, or by stress. Its consequences – sleepiness and impaired psychomotor performance – are similar to those of sleep deprivation.[56]
- Acute insomnia is the inability to consistently sleep well for a period of less than a month. Insomnia is present when there is difficulty initiating or maintaining sleep or when the sleep that is obtained is non-refreshing or of poor quality. These problems occur despite adequate opportunity and circumstances for sleep and they must result in problems with daytime function.[57] Acute insomnia is also known as short term insomnia or stress related insomnia.[58]
- Chronic insomnia lasts for longer than a month. It can be caused by another disorder, or it can be a primary disorder. People with high levels of stress hormones or shifts in the levels of cytokines are more likely than others to have chronic insomnia.[59] Its effects can vary according to its causes. They might include muscular weariness, hallucinations, and/or mental fatigue. Chronic insomnia can cause double vision.[56]
Prevention
Going to sleep and waking up at the same time every day can create a steady pattern which may help to prevent or treat insomnia.[11] Avoidance of vigorous exercise and any caffeinated drinks a few hours before going to sleep is recommended, while exercise earlier in the day is beneficial. The bedroom should be cool and dark, and the bed should only be used for sleep and sex. These are some of the points included in what doctors call “sleep hygiene“.
Treatment
It is important to identify or rule out medical and psychological causes before deciding on the treatment for insomnia.[60] Cognitive behavioral therapy (CBT) has been found to be as effective as medications for the short-term treatment of chronic insomnia. The beneficial effects, in contrast to those produced by medications, may last well beyond the stopping of therapy.[61] Medications have been used mainly to reduce symptoms in insomnia of short duration; their role in the management of chronic insomnia remains unclear.[8] Several different types of medications are also effective for treating insomnia. However, many doctors do not recommend relying on prescription sleeping pills for long-term use. It is also important to identify and treat other medical conditions that may be contributing to insomnia, such as depression, breathing problems, and chronic pain.[62]
Non-medication based
Non-medication based strategies have comparable efficacy to hypnotic medication for insomnia and they may have longer lasting effects. Hypnotic medication is only recommended for short-term use because dependence with rebound withdrawal effects upon discontinuation or tolerance can develop.[63]
Non medication based strategies provide long lasting improvements to insomnia and are recommended as a first line and long-term strategy of management. The strategies include attention to sleep hygiene, stimulus control, behavioral interventions, sleep-restriction therapy, paradoxical intention, patient education, and relaxation therapy.[64] Some examples are keeping a journal, restricting the time spent awake in bed, practicing relaxation techniques, and maintaining a regular sleep schedule and a wake-up time.[62] Behavioral therapy can assist a patient in developing new sleep behaviors to improve sleep quality and consolidation. Behavioral therapy may include, learning healthy sleep habits to promote sleep relaxation, undergoing light therapy to help with worry-reduction strategies and regulating the circadian clock.[62]
Music may improve insomnia in adults.[65] EEG biofeedback has demonstrated effectiveness in the treatment of insomnia with improvements in duration as well as quality of sleep.[66] Self-help therapy (defined as a psychological therapy that can be worked through on one’s own) may improve sleep quality for adults with insomnia to a small or moderate degree.[67]
Stimulus control therapy is a treatment for patients who have conditioned themselves to associate the bed, or sleep in general, with a negative response. As stimulus control therapy involves taking steps to control the sleep environment, it is sometimes referred interchangeably with the concept of sleep hygiene. Examples of such environmental modifications include using the bed for sleep or sex only, not for activities such as reading or watching television; waking up at the same time every morning, including on weekends; going to bed only when sleepy and when there is a high likelihood that sleep will occur; leaving the bed and beginning an activity in another location if sleep does not result in a reasonably brief period of time after getting into bed (commonly ~20 min); reducing the subjective effort and energy expended trying to fall asleep; avoiding exposure to bright light during nighttime hours, and eliminating daytime naps.[68]
A component of stimulus control therapy is sleep restriction, a technique that aims to match the time spent in bed with actual time spent asleep. This technique involves maintaining a strict sleep-wake schedule, sleeping only at certain times of the day and for specific amounts of time to induce mild sleep deprivation. Complete treatment usually lasts up to 3 weeks and involves making oneself sleep for only a minimum amount of time that they are actually capable of on average, and then, if capable (i.e. when sleep efficiency improves), slowly increasing this amount (~15 min) by going to bed earlier as the body attempts to reset its internal sleep clock. Bright light therapy, which is often used to help early morning wakers reset their natural sleep cycle, can also be used with sleep restriction therapy to reinforce a new wake schedule. Although applying this technique with consistency is difficult, it can have a positive effect on insomnia in motivated patients.
Paradoxical intention is a cognitive reframing technique where the insomniac, instead of attempting to fall asleep at night, makes every effort to stay awake (i.e. essentially stops trying to fall asleep). One theory that may explain the effectiveness of this method is that by not voluntarily making oneself go to sleep, it relieves the performance anxiety that arises from the need or requirement to fall asleep, which is meant to be a passive act. This technique has been shown to reduce sleep effort and performance anxiety and also lower subjective assessment of sleep-onset latency and overestimation of the sleep deficit (a quality found in many insomniacs).[69]
Sleep hygiene
Sleep hygiene is a common term for all of the behaviors which relate to the promotion of good sleep. These behaviors are used as the basis of sleep interventions and are the primary focus of sleep education programs.[70] Behaviors include the use of caffeine, nicotine, and alcohol consumption, maximizing the regularity and efficiency of sleep episodes, minimizing medication usage and daytime napping, the promotion of regular exercise, and the facilitation of a positive sleep environment.[70] Exercise can be helpful when establishing a routine for sleep but should not be done close to the time that you are planning on going to sleep. The creation of a positive sleep environment may also be helpful in reducing the symptoms of insomnia. In order to create a positive sleep environment one should remove objects that can cause worry or distressful thoughts from view.[citation needed]
Cognitive behavioral therapy
There is some evidence that cognitive behavioural therapy (CBT) for insomnia is superior in the long-term to benzodiazepines and the nonbenzodiazepines in the treatment and management of insomnia.[71] In this therapy, patients are taught improved sleep habits and relieved of counter-productive assumptions about sleep. Common misconceptions and expectations that can be modified include
- unrealistic sleep expectations (e.g., I need to have 8 hours of sleep each night)
- misconceptions about insomnia causes (e.g., I have a chemical imbalance causing my insomnia)
- amplifying the consequences of insomnia (e.g., I cannot do anything after a bad night’s sleep) and
- performance anxiety after trying for so long to have a good night’s sleep by controlling the sleep process.
Numerous studies have reported positive outcomes of combining cognitive behavioral therapy for insomnia treatment with treatments such as stimulus control and the relaxation therapies. Hypnotic medications are equally effective in the short-term treatment of insomnia, but their effects wear off over time due to tolerance. The effects of CBT-I have sustained and lasting effects on treating insomnia long after therapy has been discontinued.[72][73] The addition of hypnotic medications with CBT-I adds no benefit in insomnia. The long lasting benefits of a course of CBT-I shows superiority over pharmacological hypnotic drugs. Even in the short term when compared to short-term hypnotic medication such as zolpidem (Ambien), CBT-I still shows significant superiority. Thus CBT-I is recommended as a first line treatment for insomnia.[74]
Metacognition is a recent trend in approach to behaviour therapy of insomnia.[75]
Internet interventions
Despite the therapeutic effectiveness and proven success of CBT, treatment availability is significantly limited by a lack of trained clinicians, poor geographical distribution of knowledgeable professionals, and expense.[76] One way to potentially overcome these barriers is to use the Internet to deliver treatment, making this effective intervention more accessible and less costly. The Internet has already become a critical source of health-care and medical information.[77] Although the vast majority of health websites provide general information,[77][78] there is growing research literature on the development and evaluation of Internet interventions.[79][80]
These online programs are typically behaviorally-based treatments that have been operationalized and transformed for delivery via the Internet. They are usually highly structured; automated or human supported; based on effective face-to-face treatment; personalized to the user; interactive; enhanced by graphics, animations, audio, and possibly video; and tailored to provide follow-up and feedback.[80]
There is good evidence for the use computer based CBT for insomnia.[81]
Medications
Many people with insomnia use sleeping tablets and other sedatives. In some places medications are prescribed in over 95% of cases.[82] They; however, are a second line treatment.[83]
The percentage of adults using a prescription sleep aid increases with age. During 2005–2010, about 4% of U.S. adults aged 20 and over reported that they took prescription sleep aids in the past 30 days. Rates of use were lowest among the youngest age group (those aged 20–39) at about 2%, increased to 6% among those aged 50–59, and reached 7% among those aged 80 and over. More adult women (5.0%) reported using prescription sleep aids than adult men (3.1%). Non-Hispanic white adults reported higher use of sleep aids (4.7%) than non-Hispanic black (2.5%) and Mexican-American (2.0%) adults. No difference was shown between non-Hispanic black adults and Mexican-American adults in use of prescription sleep aids.[84]
Antihistamines
As an alternative to taking prescription drugs, some evidence shows that an average person seeking short-term help may find relief by taking over-the-counter antihistamines such as diphenhydramine or doxylamine.[85] Diphenhydramine and doxylamine are widely used in nonprescription sleep aids. They are the most effective over-the-counter sedatives currently available, at least in much of Europe, Canada, Australia, and the United States, and are more sedating than some prescription hypnotics.[86] Antihistamine effectiveness for sleep may decrease over time, and anticholinergic side-effects (such as dry mouth) may also be a drawback with these particular drugs. While addiction does not seem to be an issue with this class of drugs, they can induce dependence and rebound effects upon abrupt cessation of use.[citation needed] However, people whose insomnia is caused by restless legs syndrome may have worsened symptoms with antihistamines.[87]
Melatonin
The evidence for melatonin in treating insomnia is generally poor.[88] There is low quality evidence that it may speed the onset of sleep by 6 minutes.[88] Ramelteon, a melatonin receptor agonist, does not appear to speed the onset of sleep or the amount of sleep a person gets.[88]
Most melatonin drugs have not been tested for longitudinal side effects.[89] Prolonged-release melatonin may improve quality of sleep in older people with minimal side effects.[90][91]
Studies have also shown that children who are on the Autism spectrum or have learning disabilities, Attention-Deficit Hyperactivity Disorder (ADHD) or related neurological diseases can benefit from the use of melatonin. This is because they often have trouble sleeping due to their disorders. For example, children with ADHD tend to have trouble falling asleep because of their hyperactivity and, as a result, tend to be tired during most of the day. Another cause of insomnia in children with ADHD is the use of stimulants used to treat their disorder. Children who have ADHD then, as well as the other disorders mentioned, may be given melatonin before bedtime in order to help them sleep.[92]
Antidepressants
Because insomnia is a common symptom of depression, antidepressants are effective for treating sleep problems whether or not they are associated with depression. While all antidepressants help regulate sleep, some antidepressants such as amitriptyline, doxepin, mirtazapine, and trazodone can have an immediate sedative effect, and are prescribed to treat insomnia.[93] Amitriptyline and doxepin both have antihistaminergic, anticholinergic, and antiadrenergic properties, which contribute to both their therapeutic effects and side effect profiles, while mirtazapine’s side effects are primarily antihistaminergic, and trazodone’s side-effects are primarily antiadrenergic. Mirtazapine is known to decrease sleep latency (i.e., the time it takes to fall asleep), promoting sleep efficiency and increasing the total amount of sleeping time in people with both depression and insomnia.[94][95]
Agomelatine, a melatonergic antidepressant with sleep-improving qualities that does not cause daytime drowsiness,[96] is licensed for marketing in the European Union[97] and TGA Australia.[98] After trials in the United States its development for use there was discontinued in October 2011[99] by Novartis, who had bought the rights to market it there from the European pharmaceutical company Servier.[100]
Benzodiazepines
The most commonly used class of hypnotics for insomnia are the benzodiazepines.[30]:363 Benzodiazepines are not significantly better for insomnia than antidepressants.[102] Chronic users of hypnotic medications for insomnia do not have better sleep than chronic insomniacs not taking medications. In fact, chronic users of hypnotic medications have more regular nighttime awakenings than insomniacs not taking hypnotic medications.[103] Many have concluded that these drugs cause an unjustifiable risk to the individual and to public health and lack evidence of long-term effectiveness. It is preferred that hypnotics be prescribed for only a few days at the lowest effective dose and avoided altogether wherever possible, especially in the elderly.[104] Between 1993 and 2010, the prescribing of benzodiazepines to individuals with sleep disorders has decreased from 24% to 11% in the US, coinciding with the first release of nonbenzodiazepines.[105]
The benzodiazepine and nonbenzodiazepine hypnotic medications also have a number of side-effects such as day time fatigue, motor vehicle crashes and other accidents, cognitive impairments, and falls and fractures. Elderly people are more sensitive to these side-effects.[106] Some benzodiazepines have demonstrated effectiveness in sleep maintenance in the short term but in the longer term benzodiazepines can lead to tolerance, physical dependence, benzodiazepine withdrawal syndrome upon discontinuation, and long-term worsening of sleep, especially after consistent usage over long periods of time. Benzodiazepines, while inducing unconsciousness, actually worsen sleep as—like alcohol—they promote light sleep while decreasing time spent in deep sleep.[107] A further problem is, with regular use of short-acting sleep aids for insomnia, daytime rebound anxiety can emerge.[108] Although there is little evidence for benefit of benzodiazepines in insomnia compared to other treatments and evidence of major harm, prescriptions have continued to increase.[109] This is likely due to their addictive nature, both due to misuse and because—through their rapid action, tolerance and withdrawal—they can “trick” insomniacs into thinking they are helping with sleep. There is a general awareness that long-term use of benzodiazepines for insomnia in most people is inappropriate and that a gradual withdrawal is usually beneficial due to the adverse effects associated with the long-term use of benzodiazepines and is recommended whenever possible.[110][111]
Benzodiazepines all bind unselectively to the GABAA receptor.[102] Some theorize that certain benzodiazepines (hypnotic benzodiazepines) have significantly higher activity at the α1 subunit of the GABAA receptor compared to other benzodiazepines (for example, triazolam and temazepam have significantly higher activity at the α1 subunit compared to alprazolam and diazepam, making them superior sedative-hypnotics – alprazolam and diazepam, in turn, have higher activity at the α2 subunit compared to triazolam and temazepam, making them superior anxiolytic agents). Modulation of the α1 subunit is associated with sedation, motor impairment, respiratory depression, amnesia, ataxia, and reinforcing behavior (drug-seeking behavior). Modulation of the α2 subunit is associated with anxiolytic activity and disinhibition. For this reason, certain benzodiazepines may be better suited to treat insomnia than others.[citation needed]
Benzodiazepine-like medications
Drugs that may prove more effective and safer than benzodiazepines for insomnia is an area of active research.[112] Nonbenzodiazepine sedative-hypnotic drugs, such as zolpidem (Ambien), zaleplon, zopiclone (Imovane), and eszopiclone (Lunesta), are a class of hypnotic medications that are similar to benzodiazepines in their mechanism of action, and indicated for mild to moderate insomnia. Their effectiveness at improving time to sleeping is slight, and they have similar—though potentially less severe—side effect profiles compared to benzodiazepines.[113]
Suvorexant is FDA approved for insomnia, characterized by difficulties with sleep onset and/or sleep maintenance.[114]
Prescribing of nonbenzodiazepines has seen a general increase since their initial release on the US market in 1992, from 2.3% in 1993 among individuals with sleep disorders to 13.7% in 2010.[105]
Antipsychotics
The use of antipsychotics for insomnia, while common, is not recommended as the evidence does not demonstrate a benefit and the risk of adverse effects is significant.[115][116] Concerns regarding side effects is greater in the elderly.[117]
Alternative medicine
Some insomniacs use herbs such as valerian, chamomile, lavender, cannabis, hops, Withania somnifera, and passion-flower. L–Arginine L-aspartate, S-adenosyl-L-homocysteine, and delta sleep-inducing peptide (DSIP) may also be helpful in alleviating insomnia.[118] It is unclear if acupuncture is useful.[119]
Prognosis
Disability-adjusted life year for insomnia per 100,000 inhabitants in 2004.
A survey of 1.1 million residents in the United States found that those that reported sleeping about 7 hours per night had the lowest rates of mortality, whereas those that slept for fewer than 6 hours or more than 8 hours had higher mortality rates. Getting 8.5 or more hours of sleep per night was associated with a 15% higher mortality rate. Severe insomnia – sleeping less than 3.5 hours in women and 4.5 hours in men – is associated with a 15% increase in mortality.[120]
With this technique, it is difficult to distinguish lack of sleep caused by a disorder which is also a cause of premature death, versus a disorder which causes a lack of sleep, and the lack of sleep causing premature death. Most of the increase in mortality from severe insomnia was discounted after controlling for co-morbid disorders. After controlling for sleep duration and insomnia, use of sleeping pills was also found to be associated with an increased mortality rate.[120]
The lowest mortality was seen in individuals who slept between six and a half and seven and a half hours per night. Even sleeping only 4.5 hours per night is associated with very little increase in mortality. Thus, mild to moderate insomnia for most people is associated with increased longevity and severe insomnia is associated only with a very small effect on mortality.[120] It is unclear why sleeping longer than 7.5 hours is associated with excess mortality.[120]
Epidemiology
Between 10% and 30% of adults have insomnia at any given point in time and up to half of people have insomnia in a given year.[9][8][10] About 6% of people have insomnia that is not due to another problem and lasts for more than a month.[9] People over the age of 65 are affected more often than younger people.[7] Females are more often affected than males.[8] Insomnia is 40% more common in women than in men.[121]
There are higher rates of insomnia reported among university students compared to the general population.[122]
Society and culture
The topic of insomnia is discussed in many cultural contexts.[123][124]
The word insomnia is from Latin: in + somnus “without sleep” and -ia as nominalizing suffix.
The popular press have published stories about people who supposedly never sleep, such as that of Paul Kern and Al Herpin; however, these stories are not accurate.[125]
References
- “What Is Insomnia?”. NHLBI. December 13, 2011. Archived from the original on 28 July 2016. Retrieved 9 August 2016.
- “What Causes Insomnia?”. NHLBI. December 13, 2011. Archived from the original on 28 July 2016. Retrieved 9 August 2016.
- “How Is Insomnia Diagnosed?”. NHLBI. December 13, 2011. Archived from the original on 11 August 2016. Retrieved 9 August 2016.
- Watson, Nathaniel F.; Vaughn, Bradley V. (2006). Clinician’s Guide to Sleep Disorders. CRC Press. p. 10. ISBN 9780849374494.
- “How Is Insomnia Treated?”. NHLBI. December 13, 2011. Archived from the original on 28 July 2016. Retrieved 9 August 2016.
- Qaseem, A; Kansagara, D; Forciea, MA; Cooke, M; Denberg, TD; Clinical Guidelines Committee of the American College of, Physicians (3 May 2016). “Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians”. Annals of Internal Medicine. 165: 125–33. doi:10.7326/M15-2175. PMID 27136449.
- Wilson, JF (1 January 2008). “In the clinic: Insomnia”. Annals of Internal Medicine. 148 (1): ITC13–1–ITC13–16. doi:10.7326/0003-4819-148-1-200801010-01001. PMID 18166757.
- “Dyssomnias” (PDF). WHO. pp. 7–11. Archived (PDF) from the original on 2009-03-18. Retrieved 2009-01-25.
- Roth, T. (2007). “Insomnia: Definition, prevalence, etiology, and consequences”. Journal of Clinical Sleep Medicine. 3 (5 Suppl): S7–10. PMC 1978319
 . PMID 17824495.
. PMID 17824495. - Tasman, Allan; Kay, Jerald; Lieberman, Jeffrey A.; First, Michael B.; Riba, Michelle (2015). Psychiatry, 2 Volume Set (4 ed.). John Wiley & Sons. p. 4253. ISBN 9781118753361.
- Golub, R. M. (2012). “Insomnia”. JAMA. 307 (24): 2653–2653. doi:10.1001/jama.2012.6219. PMID 22735439.
- Trauer, James M.; Qian, Mary Y.; Doyle, Joseph S.; W. Rajaratnam, Shantha M.; Cunnington, David (9 June 2015). “Cognitive Behavioral Therapy for Chronic Insomnia”. Annals of Internal Medicine. 163: 191–204. doi:10.7326/M14-2841. PMID 26054060.
- Attarian, Hrayr P. (2003). Clinical Handbook of Insomnia. Springer Science & Business Media. p. Chapter 1. ISBN 9781592596621.
- Insomnia > Complications Archived 2009-02-08 at the Wayback Machine.. Mayo Clinic. Retrieved on May 5, 2009
- Consumer Reports; Drug Effectiveness Review Project (January 2012). “Evaluating New Sleeping Pills Used to Treat: Insomnia Comparing Effectiveness, Safety, and Price” (PDF). Best Buy Drugs Consumer Reports. Consumer Reports: 4. Archived (PDF) from the original on 9 December 2013. Retrieved 4 June 2013.
- Kertesz, R. S.; Cote, K. A. (2011). “Event-Related Potentials During the Transition to Sleep for Individuals with Sleep-Onset Insomnia”. Behavioral Sleep Medicine. 9 (2): 68–85. doi:10.1080/15402002.2011.557989. PMID 21491230.
- Doghramji, Karl (2007). Clinical Management of Insomnia. Caddo, OK: Professional Communications, Inc. p. 28. ISBN 978-1-932610-14-7.
- Morin, Charles (2003). Insomnia: A Clinician’s Guide to Assessment and Treatment. New York, New York: Kluwer Academic/Plenum Publishers. p. 16. ISBN 0-306-47750-5.
- “What Happens When You Sleep?”. sleepfoundation.org. Archived from the original on 2017-03-05. Retrieved 2017-02-24.
- Adler, C. H.; Thorpy, M. J. (2005). “Sleep issues in Parkinson’s disease”. Neurology. 64 (12 Suppl 3): S12–S20. doi:10.1212/WNL.64.12_suppl_3.S12. PMID 15994219.
- Harvey, A. G.; Tang, N (2011). “(Mis)Perception of Sleep in Insomnia: A puzzle and a resolution”. Psychological Bulletin. 138 (1): 77–101. doi:10.1037/a0025730. PMC 3277880
 . PMID 21967449.
. PMID 21967449. - “Insomnia”. University of Maryland Medical Center. Archived from the original on 3 July 2013. Retrieved 11 July 2013.
- Taylor, DJ; Mallory, LJ; Lichstein, KL; Durrence, HH; Riedel, BW; Bush, AJ (Feb 2007). “Comorbidity of chronic insomnia with medical problems”. Sleep. 30: 213–8. doi:10.1093/sleep/30.2.213. PMID 17326547.
- Lavie, P.; Zomer, J.; Eliaschar, I.; Joachim, Z.; Halpern, E.; Rubin, A.-H. E.; Alroy, G. (1 June 1982). “Excessive Daytime Sleepiness and Insomnia: Association With Deviated Nasal Septum and Nocturnal Breathing Disorders”. Archives of Otolaryngology – Head and Neck Surgery. 108 (6): 373–377. doi:10.1001/archotol.1982.00790540045013.
- “Insomnia Causes”. Mayo Clinic. Archived from the original on 21 October 2013. Retrieved 11 July 2013.
- “Restless Legs Syndrome/Periodic Limb Movement Disorder”. National Heart Lung and Blood Institute. Archived from the original on 3 August 2013. Retrieved 11 July 2013.
- Ramakrishnan, K.; Scheid, D. C. (2007). “Treatment options for insomnia”. American Family Physician. 76 (4): 517–526. PMID 17853625.
- Santoro, N; Epperson, CN; Mathews, SB (September 2015). “Menopausal Symptoms and Their Management”. Endocrinology and Metabolism Clinics of North America. 44 (3): 497–515. doi:10.1016/j.ecl.2015.05.001. PMC 4890704
 . PMID 26316239.
. PMID 26316239. - “What causes insomnia?”. National Heart, Lung, and Blood Institute. Archived from the original on 3 July 2013. Retrieved 11 July 2013.
- Geddes, John; Price, Jonathan; Gelder, Rebecca McKnight ; with Michael; Mayou, Richard (2012). Psychiatry (4th ed.). Oxford: Oxford University Press. ISBN 978-0199233960.
- Bendz, L. M.; Scates, A. C. (2009). “Melatonin Treatment for Insomnia in Pediatric Patients with Attention-Deficit/Hyperactivity Disorder”. Annals of Pharmacotherapy. 44 (1): 185–191. doi:10.1345/aph.1M365. PMID 20028959.
- Ouellet, M. C.; Beaulieu-Bonneau, S.; Morin, C. M. (2006). “Insomnia in patients with traumatic brain injury: Frequency, characteristics, and risk factors”. The Journal of Head Trauma Rehabilitation. 21 (3): 199–212. doi:10.1097/00001199-200605000-00001. PMID 16717498.
- Mendelson WB (2008). “New Research on Insomnia: Sleep Disorders May Precede or Exacerbate Psychiatric Conditions”. Psychiatric Times. 25 (7). Archived from the original on 2009-10-19.
- Schenkein, J.; Montagna, P. (2006). “Self management of fatal familial insomnia. Part 1: What is FFI?”. MedGenMed. 8 (3): 65. PMC 1781306
 . PMID 17406188.
. PMID 17406188. - The epidemiological survey of exercise-induced insomnia in chinese athletes Archived 2009-09-09 at the Wayback Machine. Youqi Shi, Zhihong Zhou, Ke Ning, Jianhong LIU. Athens 2004: Pre-Olympic Congress.
- Perry, Lacy. (2004-10-12) HowStuffWorks “How Hangovers Work” Archived 2010-03-15 at the Wayback Machine.. Health.howstuffworks.com. Retrieved on 2011-11-20.
- Lee-chiong, Teofilo (24 April 2008). Sleep Medicine: Essentials and Review. Oxford University Press, USA. p. 105. ISBN 0-19-530659-7.
- Ashton, Heather (2005-05-01). “The diagnosis and management of benzodiazepine dependence”. Current Opinion in Psychiatry. 18 (3): 249–255. doi:10.1097/01.yco.0000165594.60434.84. PMID 16639148.
- Morin, Charles M.; Bélanger, Lynda; Bastien, Célyne; Vallières, Annie (2005-01-01). “Long-term outcome after discontinuation of benzodiazepines for insomnia: a survival analysis of relapse”. Behaviour Research and Therapy. 43 (1): 1–14. doi:10.1016/j.brat.2003.12.002. PMID 15531349.
- Poyares, Dalva; Guilleminault, Christian; Ohayon, Maurice M.; Tufik, Sergio (2004-06-01). “Chronic benzodiazepine usage and withdrawal in insomnia patients”. Journal of Psychiatric Research. 38 (3): 327–334. doi:10.1016/j.jpsychires.2003.10.003. PMID 15003439.
- Asaad, T. A.; Ghanem, M. H.; Abdel Samee, A. M.; El–Habiby, M. M. (2011). “Sleep Profile in Patients with Chronic Opioid Abuse”. Addictive Disorders & Their Treatment. 10: 21–28. doi:10.1097/ADT.0b013e3181fb2847.
- Roth, Thomas (15 August 2007). “Insomnia: Definition, Prevalence, Etiology, and Consequences”. Journal of Clinical Sleep Medicine. 3 (5 Suppl): S7–S10. PMC 1978319
 . PMID 17824495.
. PMID 17824495. - Bonnet, Michael H. (1 April 2009). “Evidence for the Pathophysiology of Insomnia”. Sleep. 32 (4): 441–442. doi:10.1093/sleep/32.4.441. PMC 2663857
 . PMID 19413138.
. PMID 19413138. - Levenson, Jessica C.; Kay, Daniel B.; Buysse, Daniel J. (22 January 2017). “The Pathophysiology of Insomnia”. Chest. 147 (4): 1179–1192. doi:10.1378/chest.14-1617. PMC 4388122
 . PMID 25846534.
. PMID 25846534. - Mai, Evelyn; Buysse, Daniel J. (1 January 2008). “Insomnia: Prevalence, Impact, Pathogenesis, Differential Diagnosis, and Evaluation”. Sleep Medicine Clinics. 3 (2): 167–174. doi:10.1016/j.jsmc.2008.02.001. PMC 2504337
 . PMID 19122760.
. PMID 19122760. - Shaver, JL; Woods, NF (August 2015). “Sleep and menopause: a narrative review”. Menopause. 22 (8): 899–915. doi:10.1097/GME.0000000000000499. PMID 26154276.
- Lord, C; Sekerovic, Z; Carrier, J (October 2014). “Sleep regulation and sex hormones exposure in men and women across adulthood”. Pathologie-biologie. 62 (5): 302–10. doi:10.1016/j.patbio.2014.07.005. PMID 25218407.
- Soldatos, CR; Dikeos, DG; Paparrigopoulos, TJ (Jun 2000). “Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria”. Journal of Psychosomatic Research. 48: 555–560. doi:10.1016/S0022-3999(00)00095-7. PMID 11033374.
- Passarella, S, Duong, M. “Diagnosis and treatment of insomnia.” 2008.
- Schutte-Rodin, Sharon; Broch, Lauren; Buysse, Daniel; Dorsey, Cynthia; Sateia, Michael (2015). “Clinical Guideline for the Evaluation and Management of Chronic Insomnia in Adults” (PDF). Journal of Clinical Sleep Medicine. AASM. p. 488. Archived (PDF) from the original on 9 February 2015. Retrieved 30 July 2015.
Actigraphy is indicated as a method to characterize circadian patterns or sleep disturbances in individuals with insomnia, …
- American College of Occupational and Environmental Medicine (February 2014), “Five Things Physicians and Patients Should Question”, Choosing Wisely: an initiative of the ABIM Foundation, American College of Occupational and Environmental Medicine, archived from the original on 11 September 2014, retrieved 24 February 2014
- Thorpy, Michael J. (October 2012). “Classification of Sleep Disorders”. Neurotherapeutics. 9 (4): 687–701. doi:10.1007/s13311-012-0145-6. PMC 3480567
 . PMID 22976557.
. PMID 22976557. - Wilson, S.; Nutt, D.; Alford, C.; Argyropoulos, S.; Baldwin, D.; Bateson, A.; Britton, T.; Crowe, C.; Dijk, D. -J.; Espie, C.; Gringras, P.; Hajak, G.; Idzikowski, C.; Krystal, A.; Nash, J.; Selsick, H.; Sharpley, A.; Wade, A. (2010). “British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders”. Journal of Psychopharmacology. 24 (11): 1577–1601. doi:10.1177/0269881110379307. PMID 20813762.
- Luca, A; Luca, M; Calandra, C (2013). “Sleep disorders and depression: brief review of the literature, case report, and nonpharmacologic interventions for depression”. Clinical Interventions in Aging. 8: 1033–9. doi:10.2147/CIA.S47230. PMC 3760296
 . PMID 24019746.
. PMID 24019746. - “Sleep Wake Disorders .” Diagnostic and statistical manual of mental disorders: DSM-5.. 5th ed. Washington, D.C.: American Psychiatric Association, 2013. -. Print.
- Roth, T.; Roehrs, T. (2003). “Insomnia: Epidemiology, characteristics, and consequences”. Clinical Cornerstone. 5 (3): 5–15. doi:10.1016/S1098-3597(03)90031-7. PMID 14626537.
- “Insomnia – sleeplessness, chronic insomnia, acute insomnia, mental ..” Archived from the original on March 29, 2008. Retrieved 2008-04-29.
- “Acute Insomnia – What is Acute Insomnia”. Sleepdisorders.about.com. Archived from the original on 2013-03-29. Retrieved 2013-03-10.
- Simon, Harvey. “In-Depth Report: Causes of Chronic Insomnia”. New York Times. Archived from the original on 8 November 2011. Retrieved 4 November 2011.
- Wortelboer, U.; Cohrs, S.; Rodenbeck, A.; Rüther, E. (2002). “Tolerability of hypnosedatives in older patients”. Drugs & Aging. 19 (7): 529–539. doi:10.2165/00002512-200219070-00006. PMID 12182689.
- “NIH State-of-the-Science Conference Statement on manifestations and management of chronic insomnia in adults”. NIH Consensus and State-of-the-Science Statements. 22 (2): 1–30. 2005. PMID 17308547.
- Merrigan, Jill M.; Buysse, Daniel J.; Bird, Joshua C.; Livingston, Edward H. (2013). “Insomnia”. JAMA. 309 (7): 733. doi:10.1001/jama.2013.524. PMID 23423421. Archived from the original on 2013-05-29.
- National Prescribing Service (2010-02-01). “Addressing hypnotic medicines use in primary care” Archived 2013-11-01 at the Wayback Machine.. NPS News, Vol 67.
- Kirkwood, C. K. (1999). “Management of insomnia”. Journal of the American Pharmaceutical Association. 39 (5): 688–696; quiz 696–4. PMID 10533351.
- Jespersen, KV; Koenig, J; Jennum, P; Vuust, P (13 August 2015). “Music for insomnia in adults”. The Cochrane Database of Systematic Reviews. 8: CD010459. doi:10.1002/14651858.CD010459.pub2. PMID 26270746.
- Lake, James A. (31 October 2006). Textbook of Integrative Mental Health Care. Thieme Medical Publishers. p. 313. ISBN 1-58890-299-4.
- van Straten, A; Cuijpers, P (February 2009). “Self-help therapy for insomnia: a meta-analysis”. Sleep Medicine Reviews. 13 (1): 61–71. doi:10.1016/j.smrv.2008.04.006. PMID 18952469.
- Lande, R. G.; Gragnani, C. (2010). “Nonpharmacologic approaches to the management of insomnia”. The Journal of the American Osteopathic Association. 110 (12): 695–701. PMID 21178150.
- Kierlin, L (November 2008). “Sleeping without a pill: nonpharmacologic treatments for insomnia”. Journal of Psychiatric Practice. 14 (6): 403–7. doi:10.1097/01.pra.0000341896.73926.6c. PMID 19057243.
- Ellis, J. J., Hampson, S. E., & Cropley, M. M. “Sleep hygiene or compensatory sleep practices: an examination of behaviors affecting sleep in older adults”. 2002
- Mitchell, M. D.; Gehrman, P.; Perlis, M.; Umscheid, C. A. (2012). “Comparative effectiveness of cognitive behavioral therapy for insomnia: A systematic review”. BMC Family Practice. 13: 40. doi:10.1186/1471-2296-13-40. PMC 3481424
 . PMID 22631616. Archived from the original on 2016-03-04.
. PMID 22631616. Archived from the original on 2016-03-04. - Jacobs, G. D.; Pace-Schott, E. F.; Stickgold, R.; Otto, M. W. (2004). “Cognitive behavior therapy and pharmacotherapy for insomnia: a randomized controlled trial and direct comparison” (PDF). Archives of Internal Medicine. 164 (17): 1888–1896. doi:10.1001/archinte.164.17.1888. PMID 15451764. Archived from the original (PDF) on 2012-12-22.
- Morin, C. M.; Colecchi, C.; Stone, J.; Sood, R.; Brink, D. (1999). “Behavioral and pharmacological therapies for late-life insomnia: A randomized controlled trial”. JAMA. 281 (11): 991–999. doi:10.1001/jama.281.11.991. PMID 10086433.
- Miller, K. E. (2005). “Cognitive Behavior Therapy vs. Pharmacotherapy for Insomnia”. American Family Physician. Archived from the original on 2011-06-06.
- Ong, J. C.; Ulmer, C. S.; Manber, R. (2012). “Improving sleep with mindfulness and acceptance: A metacognitive model of insomnia”. Behaviour Research and Therapy. 50 (11): 651–660. doi:10.1016/j.brat.2012.08.001. PMC 3466342
 . PMID 22975073.
. PMID 22975073. - Edinger, J. D.; Means, M. K. (2005). “Cognitive–behavioral therapy for primary insomnia”. Clinical Psychology Review. 25 (5): 539–558. doi:10.1016/j.cpr.2005.04.003. PMID 15951083.
- Fox S, Fallows D. (2005-10-05) Internet health resources. Washington, DC: Pew Internet & American Life Project; 2003.
- Rabasca L. (2000). “Taking telehealth to the next step”. Monitor on Psychology. 31: 36–37. doi:10.1037/e378852004-017. Archived from the original on 2012-12-30.
- Marks IM, Cavanagh K, Gega L. (2007) Hands-on Help: Computer-Aided Psychotherapy. Hove, England and New York: Psychology Press, ISBN 184169679X.
- Ritterband, L. M.; Gonder-Frederick, L. A.; Cox, D. J.; Clifton, A. D.; West, R. W.; Borowitz, S. M. (2003). “Internet interventions: In review, in use, and into the future”. Professional Psychology: Research and Practice. 34 (5): 527–534. doi:10.1037/0735-7028.34.5.527.
- Cheng, SK; Dizon, J (2012). “Computerised cognitive behavioural therapy for insomnia: a systematic review and meta-analysis”. Psychotherapy and Psychosomatics. 81 (4): 206–16. doi:10.1159/000335379. PMID 22585048.
- Harrison C, Britt H (2009). “Insomnia” (PDF). Australian Family Physician. 32: 283. Archived (PDF) from the original on 2011-03-12.
- Qaseem, A; Kansagara, D; Forciea, MA; Cooke, M; Denberg, TD; Clinical Guidelines Committee of the American College of, Physicians (19 July 2016). “Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians”. Annals of Internal Medicine. 165 (2): 125–33. doi:10.7326/m15-2175. PMID 27136449.
- Chong Y., Fryar, C.D., and Gu, Q. (2013). Prescription Sleep Aid Use Among Adults: United States, 2005–2010. Hyattsville, Md.: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
- Consumer Reports; Drug Effectiveness Review Project (January 2012). “Evaluating Newer Sleeping Pills Used to Treat: Insomnia. Comparing Effectiveness, Safety, and Price” (PDF). Best Buy Drugs. Consumer Reports: 3, 8, 11. Archived (PDF) from the original on 9 December 2013. Retrieved 4 June 2013.
- DrugBank: DB00366 (Doxylamine) Archived 2009-12-03 at the Wayback Machine.. Drugbank.ca. Retrieved on 2011-11-20.
- “Restless Legs Syndrome Fact Sheet | National Institute of Neurological Disorders and Stroke”. www.ninds.nih.gov. Archived from the original on 28 July 2017. Retrieved 29 August 2017.
- Brasure, M; MacDonald, R; Fuchs, E; Olson, CM; Carlyle, M; Diem, S; Koffel, E; Khawaja, IS; Ouellette, J; Butler, M; Kane, RL; Wilt, TJ (December 2015). “Management of Insomnia Disorder”. PMID 26844312.
- Conn, D. K.; Madan, R. (2006). “Use of Sleep-Promoting Medications in Nursing Home Residents”. Drugs & Aging. 23 (4): 271–287. doi:10.2165/00002512-200623040-00001. PMID 16732687.
- Lyseng-Williamson, KA (November 2012). “Melatonin prolonged release: in the treatment of insomnia in patients aged ≥55 years”. Drugs & Aging. 29 (11): 911–23. doi:10.1007/s40266-012-0018-z. PMID 23044640.
- Lemoine, P; Zisapel, N (April 2012). “Prolonged-release formulation of melatonin (Circadin) for the treatment of insomnia”. Expert Opinion on Pharmacotherapy. 13 (6): 895–905. doi:10.1517/14656566.2012.667076. PMID 22429105.
- Sánchez-Barceló, Emilio; Mediavilla, Maria; Reiter, Russel J. (2011). “Clinical Uses of Melatonin in Pediatrics”. International Journal of Pediatrics. 2011: 1–11. doi:10.1155/2011/892624.
- Bertschy, G.; Ragama-Pardos, E.; Muscionico, M.; Aït-Ameur, A.; Roth, L.; Osiek, C.; Ferrero, F. O. (2005). “Trazodone addition for insomnia in venlafaxine-treated, depressed inpatients: A semi-naturalistic study”. Pharmacological Research. 51 (1): 79–84. doi:10.1016/j.phrs.2004.06.007. PMID 15519538.
- Winokur, A.; Demartinis Na, 3.; McNally, D. P.; Gary, E. M.; Cormier, J. L.; Gary, K. A. (2003). “Comparative effects of mirtazapine and fluoxetine on sleep physiology measures in patients with major depression and insomnia”. The Journal of Clinical Psychiatry. 64 (10): 1224–1229. doi:10.4088/JCP.v64n1013. PMID 14658972.
- Schittecatte, M.; Dumont, F.; Machowski, R.; Cornil, C.; Lavergne, F.; Wilmotte, J. (2002). “Effects of mirtazapine on sleep polygraphic variables in major depression”. Neuropsychobiology. 46 (4): 197–201. doi:10.1159/000067812. PMID 12566938.
- Strat YL; Gorwood, P (September 2008). “Agomelatine, an innovative pharmacological response to unmet needs”. Journal of Psychopharmacology. 22 (suppl. 7): 4–8. doi:10.1177/0269881108092593. PMID 18753276.
- “Summary of Product Characteristics” (PDF). European Medicine Agency. Archived (PDF) from the original on 2014-10-29. Retrieved 2013-10-14.
- “VALDOXAN® Product Information” (PDF). TGA eBusiness Services. Servier Laboratories Pty Ltd. 2013-09-23. Archived from the original on 2017-03-24. Retrieved 2013-10-14.
- Novartis drops future blockbuster agomelatine. Archived 2011-11-11 at the Wayback Machine. Scrip Intelligence, Oct 25 2011 (retrieved Oct 30, 2011).
- Bentham, Clara (2006-03-29). “Servier and Novartis sign licensing agreement for agomelatine, a novel treatment for depression”. Servier UK. Archived from the original on 16 April 2009. Retrieved 2009-05-15.
- Temazepam Archived 2013-05-30 at the Wayback Machine.. Websters-online-dictionary.org. Retrieved on 2011-11-20.
- Buscemi, N.; Vandermeer, B.; Friesen, C.; Bialy, L.; Tubman, M.; Ospina, M.; Klassen, T. P.; Witmans, M. (2007). “The Efficacy and Safety of Drug Treatments for Chronic Insomnia in Adults: A Meta-analysis of RCTs”. Journal of General Internal Medicine. 22 (9): 1335–1350. doi:10.1007/s11606-007-0251-z. PMC 2219774
 . PMID 17619935.
. PMID 17619935. - Ohayon, M. M.; Caulet, M. (1995). “Insomnia and psychotropic drug consumption”. Progress in Neuro-psychopharmacology & Biological Psychiatry. 19 (3): 421–431. doi:10.1016/0278-5846(94)00023-B. PMID 7624493.
- “What’s wrong with prescribing hypnotics?”. Drug and Therapeutics Bulletin. 42 (12): 89–93. 2004. doi:10.1136/dtb.2004.421289. PMID 15587763.
- Kaufmann, Christopher N.; Spira, Adam P.; Alexander, G. Caleb; Rutkow, Lainie; Mojtabai, Ramin (2015). “Trends in prescribing of sedative-hypnotic medications in the USA: 1993–2010”. Pharmacoepidemiology and Drug Safety. 25 (6): 637–45. doi:10.1002/pds.3951. PMC 4889508
 . PMID 26711081. Archived from the original on 2016-06-09.
. PMID 26711081. Archived from the original on 2016-06-09. - Glass, J.; Lanctôt, K. L.; Herrmann, N.; Sproule, B. A.; Busto, U. E. (2005). “Sedative hypnotics in older people with insomnia: Meta-analysis of risks and benefits”. BMJ. 331 (7526): 1169. doi:10.1136/bmj.38623.768588.47. PMC 1285093
 . PMID 16284208.
. PMID 16284208. - Tsoi, W. F. (1991). “Insomnia: Drug treatment”. Annals of the Academy of Medicine, Singapore. 20 (2): 269–272. PMID 1679317.
- Montplaisir, J. (2000). “Treatment of primary insomnia”. Canadian Medical Association Journal. 163 (4): 389–391. PMC 80369
 . PMID 10976252.
. PMID 10976252. - Carlstedt, Roland A. (13 December 2009). Handbook of Integrative Clinical Psychology, Psychiatry, and Behavioral Medicine: Perspectives, Practices, and Research. Springer. pp. 128–130. ISBN 0-8261-1094-0.
- Lader, Malcolm Harold; P. Cardinali, Daniel; R. Pandi-Perumal, S. (22 March 2006). Sleep and sleep disorders: a neuropsychopharmacological approach. Georgetown, Tex.: Landes Bioscience/Eurekah.com. p. 127. ISBN 0-387-27681-5.
- Authier, N.; Boucher, A.; Lamaison, D.; Llorca, P. M.; Descotes, J.; Eschalier, A. (2009). “Second Meeting of the French CEIP (Centres d’Évaluation et d’Information sur la Pharmacodépendance). Part II: Benzodiazepine Withdrawal”. Thérapie. 64 (6): 365–370. doi:10.2515/therapie/2009051. PMID 20025839.
- Rosenberg, R. P. (2006). “Sleep Maintenance Insomnia: Strengths and Weaknesses of Current Pharmacologic Therapies”. Annals of Clinical Psychiatry. 18 (1): 49–56. doi:10.1080/10401230500464711. PMID 16517453.
- Huedo-Medina, T. B.; Kirsch, I.; Middlemass, J.; Klonizakis, M.; Siriwardena, A. N. (2012). “Effectiveness of non-benzodiazepine hypnotics in treatment of adult insomnia: Meta-analysis of data submitted to the Food and Drug Administration”. BMJ. 345: e8343. doi:10.1136/bmj.e8343. PMC 3544552
 . PMID 23248080.
. PMID 23248080. - “Highlights of prescribing information” (PDF). Archived (PDF) from the original on 2014-09-12.
- American Psychiatric Association (September 2013), “Five Things Physicians and Patients Should Question”, Choosing Wisely: an initiative of the ABIM Foundation, American Psychiatric Association, archived from the original on 3 December 2013, retrieved 30 December 2013, which cites
- ADA, APA, AACE, and NAASO (1 February 2004). “Consensus Development Conference on Antipsychotic Drugs and Obesity and Diabetes”. Diabetes Care. 27 (2): 596–601. doi:10.2337/diacare.27.2.596. PMID 14747245.
- Maglione, M; Maher, AR; Hu, J; Wang, Z; Shanman, R; Shekelle, PG; Roth, B; Hilton, L; Suttorp, MJ; Ewing, BA; Motala, A; Perry, T (Sep 2011). “Off-Label Use of Atypical Antipsychotics: An Update”. PMID 22132426.
- Nasrallah, HA (Jan 2008). “Atypical antipsychotic-induced metabolic side effects: insights from receptor-binding profiles”. Molecular Psychiatry. 13 (1): 27–35. doi:10.1038/sj.mp.4002066. PMID 17848919.
- Coe, HV; Hong, IS (May 2012). “Safety of low doses of quetiapine when used for insomnia”. The Annals of Pharmacotherapy. 46 (5): 718–22. doi:10.1345/aph.1Q697. PMID 22510671.
- Conn, DK; Madan, R (2006). “Use of sleep-promoting medications in nursing home residents : risks versus benefits”. Drugs & Aging. 23 (4): 271–87. doi:10.2165/00002512-200623040-00001. PMID 16732687.
- Billiard M, Kent A (2003). Sleep: physiology, investigations, medicine. pp. 275–7. ISBN 978-0-306-47406-4.
- Cheuk, DK; Yeung, WF; Chung, KF; Wong, V (12 September 2012). “Acupuncture for insomnia”. The Cochrane Database of Systematic Reviews. 9 (9): CD005472. doi:10.1002/14651858.CD005472.pub3. hdl:10722/198790. PMID 22972087.
- Kripke, D. F.; Garfinkel, L.; Wingard, D. L.; Klauber, M. R.; Marler, M. R. (2002). “Mortality associated with sleep duration and insomnia”. Archives of General Psychiatry. 59 (2): 131–136. doi:10.1001/archpsyc.59.2.131. PMID 11825133.
- “Several Sleep Disorders Reflect Gender Differences”. Psychiatric News. 42 (8): 40. 2007.
- Jiang, X.-l; Zheng, X.-y; Yang, J.; Ye, C.-p; Chen, Y.-y; Zhang, Z.-g; Xiao, Z.-j (2015-12-01). “A systematic review of studies on the prevalence of insomnia in university students”. Public Health. 129 (12): 1579–1584. doi:10.1016/j.puhe.2015.07.030. PMID 26298588.
- Summers-Bremner, Eluned (2010). Insomnia: A cultural history. London: Reaktion. ISBN 1861896549.
- Brigitte Steger (2009). “Insomnia: A Cultural History (review)”. Bulletin of the History of Medicine. 83 (2): 385–386. doi:10.1353/bhm.0.0210.
Jim., Horne, (2016). Sleeplessness Assessing Sleep Need in Society Today. p. 114. ISBN 9783319305721.